Abstract
Background: Measurable residual disease (MRD) status pre-allogeneic stem cell transplantation (alloSCT) has been shown to predict outcome after transplant. Nonetheless, the impact of MRD persistence pre-alloSCT (MRD+) on transplant outcome might be modulated by relevant procedure features, such as conditioning intensity (Am J Hem 2018) or the use of anti thymocyte globulin (ATG) to prevent chronic graft versus host disease (cGVHD). Thus, since cGVHD is associated with graft versus leukemia effect (GVL), there is a concern that ATG may hamper GVL and increase relapse after transplant, especial in patients (pts) with a higher risk such as MRD+. For this purpose, we investigated whether MRD status pre-alloSCT modifies the effect of ATG on AML relapse post alloSCT in a large cohort of pts undergoing alloSCT in CR1, adjusting for other important variables on outcome.
Methods: Inclusion criteria were adult AML pts with intermediate or adverse risk cytogenetics according to MRC and known FLT3-ITD status undergoing alloSCT in CR1 from either a HLA matched sibling (MSD) or (10/10) matched unrelated donors (MUD) during 2006-2017 period. First, we assessed the impact of MRD status, cytogenetics, FLT3-ITD and ATG as part of the conditioning in the whole population. Then, we studied the impact of ATG in accordance to MRD status at time of transplantation. Results are given at 2 years.
Results: 1509 pts (1083 MRD negative (MRD-) and 426 MRD+) met the inclusion criteria. In the MRD- group, 552 (48%) pts did not receive ATG and 561 (52%) received ATG, whereas within MRD+ cohort, 187 (44%) received no ATG and 239 (58%) received ATG. Median age was 51 (range 18-73) years, 51% were females. Median year of alloSCT was 2014; 85% and 15% of the pts harbored intermediate and adverse risk cytogenetics, respectively. FLT3-ITD was identified in 51% of the pts, and NPM1 was mutated in 689 (56%). 59% of the pts underwent alloSCT from MSD while 41% from MUD. 82% of the pts received PB grafts; 58% received myeloablative (MAC) while 42% reduced intensity conditioning (RIC). The GVHD prophylaxis was CSA/MTX followed by CSA/MMF in the majority of the pts (75 %). 24% of pts developed grade II-IV while 7% grade III-IV acute (a) GVHD. cGVHD occurred in 30% of the pts, being extensive in half of them.
In the overall population, aGVHD grade III-IV, cGVHD total and extensive were significantly lower in pts who received ATG in comparison to those who did not (6% vs 9%, p=0.04; 30% vs 45%, p<10-5; 15% vs 25%, p<10-4, respectively), translating into better GVHD-relapse-free survival (GRFS; 52% vs 43%, p=0.007). Non relapse mortality (NRM), relapse (RI), leukemia-free survival (LFS) and overall survival (OS) did not differ statistically between pts who received or did not receive ATG. Focusing on the influence of MRD status, RI was higher in MRD+ (39% vs. 23%, p<10-5), and LFS, OS and GRFS were all significantly superior in the MRD- cohort (66% vs 51% p<10-5; 73% vs 60% p=<10-5 and 51% vs 37% p<10-5, respectively). In contrast, NRM and GVHD did not differ between the groups.
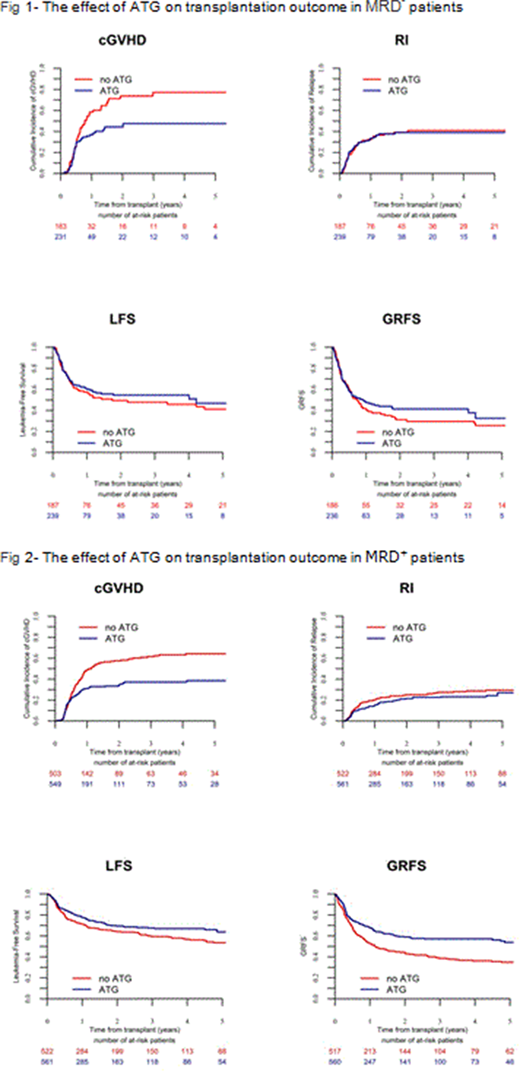
Then, we investigated the effect of ATG separately in MRD- and MRD+pts. By multivariate analysis, in MRD- pts, ATG did not affect RI (24% vs. 21% in no ATG and ATG; HR 0.80, P=0.17), but was associated with lower incidence of grade II-IV aGVHD, grade III-IV aGVHD, cGVHD, extensive cGVHD and NRM (HR 0.71 P=0.04, HR 0.37 P<10-3; HR 0.55 p<10-4, HR 0.42 P<10-4 and HR 0.66 p=0.05, respectively). As a consequence, ATG was associated with improved LFS, OS and GRFS (HR 0.74 P=0.02, HR 0.69 P=0.01 and HR 0.62 P<10-3). In MRD+ pts, ATG was associated with lower incidence of cGVHD and extensive cGVHD (HR 0.56 p= 0.03, HR 0.40 P=0.01, respectively), without a significant impact on any other alloSCT outcome parameters, including RI (39% vs 39% in no ATG and ATG; HR 1.02 P=0.92). FLT3 was associated with a higher RI in both MRD- and MRD+ pts. Finally, in both MRD- and MRD+groups, there was no interaction between ATG and cytogenetics, FLT3 and donor type as neither of these 3 factors influenced significantly the effect of ATG.
Conclusions: ATG reduces severe (grade II-IV) acute and both chronic and extensive chronic GVHD in AML pts undergoing alloSCT in CR1, resulting in improved GRFS. Most importantly, the clinical benefit of ATG in terms of GVHD prevention was not achieved at the expense of an increased relapse incidence including in MRD+ pts pre-alloSCT.
Mohty:MaaT Pharma: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal